Dr. Brian Van Tine and Dr. Charles Schutt from Washington University in St. Louis discuss their 2021 research published by Oncotarget, entitled, “Genomic and neoantigen evolution from primary tumor to first metastases in head and neck squamous cell carcinoma.”
Behind the Study is a series of transcribed videos from researchers elaborating on their oncology-focused studies published by Oncotarget. Visit the Oncotarget YouTube channel for more insights from outstanding authors.
—
Hi, I’m Brian Van Tine, I am the phase one co-director at Washington University in St. Louis and the Siteman Cancer Center, and I am greatly going to happily be joined today by an ex-postdoc of mine who just put out a very important paper, named Charles Schutt.
Hi, I’m Dr. Charles Schutt. I was Dr. Van Tine’s lab manager, staff scientist, second in command, hand of the king, whatever it needed to be.
Dr. Brian Van Tine
We worked really, really hard in collaboration with Columbia University and Li Ding‘s group to actually put together a paper on making neoantigen evolution, of what happens in a head and neck cancer when you go from a primary tumor to first metastasis. And we looked at neoantigens, we looked at genetic evolution, and we learned quite a lot doing this. Wouldn’t you say, Charles?
Dr. Charles Schutt
We definitely learned a lot doing this.
Dr. Brian Van Tine
And that cancer’s one of those cancers that represents about 3% of all cancers, but it’s associated with events that happen during your lifetime. It’s associated with human papillomavirus, it’s associated with drinking and smoking, and this leads to a lot of DNA damage. So it’s an interesting tumor, it’s a tumor that’s in need of new therapies. It’s a tumor that’s in need of really a different view of understanding, and so Charles led a team that looked at some very important samples we actually had in our tumor bank.
Dr. Charles Schutt
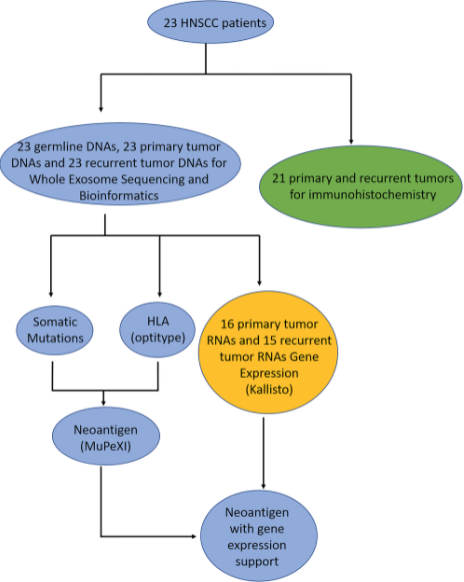
So this was a fun project for me to step into. Dr. Ding’s lab had already done a lot of the work isolating and doing all of the omic analysis, so looking at the DNA mutations over time, looking at RNA sequencing over time, predicting neoantigens over time. And I got to step into this and say, “Okay, we have all of this information. We have all of that, and we have this immunohistic chemistry data from Dr. Ingham’s group at Columbia University. What does it mean?” So that was very fun to take all of this and put together this story in our publication.
Dr. Brian Van Tine
We can forget that Doug Adkins, 15 years ago, had the idea to start banking what he was doing. And so he runs a very large head and neck cancer clinic, and he was banking primary tumors, and then he would be biopsying first metastases to prove it was cancer, and all this was banked. Out of this became a really unique set of agents. We actually had 23 patients where we had not only the first primary tumor, but then we had outcomes data for when they actually metastasized, where they arose from, and what their genomics were. I think this really began to give us a unique tool to really look at this from a different way.
Dr. Charles Schutt
Definitely so.
Dr. Brian Van Tine
I think what was neat about Charles’ background is he’s actually a really well-trained immunologist, and he really began to piece together immunology of what was going on, patient by patient. It’s not a large dataset, but we contacted other institutions looking for similar paired consented patients, and they’re really hard to find. Even in the modern day and age where we’re doing this perspectively, this is our first glimpse in head and neck cancer where you actually get an idea of what’s going on.
Dr. Charles Schutt
At least to our knowledge, this is the first study where anyone has looked at paired samples and actually tried to predict neoantigen burdens and neoantigen changes over time. So it was very exciting for us to be able to pair that data with mutation data and with all of the other things we were able to do in this study.
Dr. Brian Van Tine
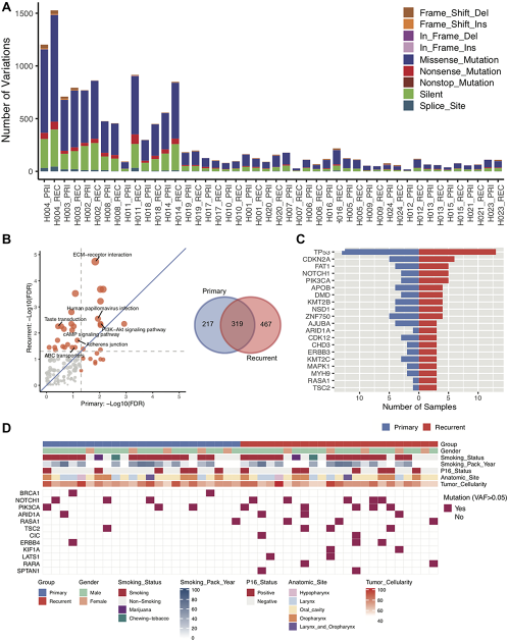
I think what what was kind of the most striking thing you’d showed me is when we started seeing neoantigens, not necessarily at the same place in the same genes, but within recurrent genes, up to what? Four or five different patients, the same gene that was evolving between the primary and the metastasis? When you think of that we only had 23 samples, I think there’s an insight, or at least a beginning of a hint, that there’s pathways that get activated as you know, and we assume. But there’s this neoantigen evolution as you need to escape the immune system once your primary tumor is gone to establish a new home and then to actually grow it later.
Dr. Charles Schutt
Well, and what was exciting to us, not only were we seeing these mutations occurring in the same genes, that actually seemed to be correlating with outcomes. When patients had mutations in these genes, they had these predicted neoantigens. This seemed to be correlating with them living longer, having more T-cell infiltration into the tumor. Positive things for the patient, so it was very exciting for us and hopefully interesting stuff forward for the field.
Dr. Brian Van Tine
I think one of the things that struck me is one of the genes that seems to get hit a lot is actually pi3 kinase, and that biology and the changes in that kinase may be much more important than we thought in terms of just directly drugging it. So if we can begin to understand more of this process that’s happening actually in my favorite animal model, which is people, maybe we can use this against the tumor. I think we need larger data sets. I think we need to be able to do this on a much bigger scale. But the hints into this, it’s not breast cancer in terms of the number of patients who get this. It’s more of a rare disease, but it’s not as rare as some of the other diseases I actually treat. But there’s a hint here that I think there’s something special, and your really unique look into the infiltrates and the work you did with Columbia. I think really is something you should discuss.
Dr. Charles Schutt
What was very interesting for us is, like we said, there were these recurrent mutation in genes, and this seemed to be correlating with an increase in CD8 T cell infiltration. We seem to be seeing an increase in cytolytic activity, at least on the transcript level within these tumors as well, which was very interesting and exciting for us. Our samples had a bit of a limitation in that they’re banked, so we really didn’t have anything to come back to to actually verify whether the neoantigens we were predicting are actual neoantigens, but that would be an interesting step forward to see how these predictions are playing out in the tumor.
Dr. Brian Van Tine
I think this is the direction that needs to happen next, because if we actually can find subgroups of recurrent genes to go after, this may start helping us take apart a disease that’s not just one disease, but many, many, many different diseases with many, many different subsets. So I think you should be very proud of this work you led.
Dr. Charles Schutt
I know. This was fantastic collaborative effort from a lot of different people with a lot of different backgrounds, but it was exciting to put together. It was exciting to work with many different people across many different places. And even in a challenging time where we’re all working remotely, it was quite the accomplishment to get all of this put together and out and published.
Dr. Brian Van Tine
I think it’s important to always thank our funders, who had the foresight to know that this was going to be interesting and potentially transformative. The actual division of medical oncology at Washington University where John DiPersio really does support us, and just our philanthropy support orders. So from that standpoint, I also want to thank Li Ding for all the hard work of her group, and a group that came together from Columbia that really did make things happen in a way that I thought was really, really nice. Do you have any closing thoughts, Charles?
Dr. Charles Schutt
I’d also like to thank that patients who were willing to let their samples be biopsied and banked for this study. We could not do this without them, so we’re very grateful to have patients that are willing to participate with us.
Dr. Brian Van Tine
I look forward to elaborating. Charles moved to Japan just to escape me, and so he’s direly missed. But I look forward to continuing this work, both here and in Japan, and seeing if we can actually make this discovery a transformative thing for patients. So thank you for joining me, whether it’s really late or really early.
Dr. Charles Schutt
It’s a little bit of both in Japan, but thank you for letting me join in on this. This has been a lot of fun, and it’s a lot of fun to talk about. This was really exciting work for us, and it’s glad to see that it got published, that it’s getting some push from Oncotarget. It’s been a quite the experience.
Dr. Brian Van Tine
We also want to thank the editors of Oncotarget for allowing us the ability to talk about this. And thank you if you’ve made it to the end of the recording for listening. Thank you very much.
Dr. Charles Schutt
Thank you.
Click here to read the full study published by Oncotarget.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.